Breathing
1.7.2. Breathing
Most newly born infants will make vigorous efforts to breathe at birth.
|
Positive pressure ventilation devices:
The Australian and New Zealand Resuscitation Committee on Resuscitation (ANZCOR) state:
“A T-piece resuscitator device, a self inflating bag (approximately 240mL), and a flow inflating bag are all acceptable devices to ventilate newborn infants either via a face mask, supraglottic airway (laryngeal mask) or endotracheal tube” (ANZCOR 2021, Guideline 13.4).
Each manual ventilation device has its own unique advantages and limitations, which are discussed below.
1. T-piece device (Neopuff™ , NeoPIP™ or similar device)

F & P Neopuff™ Infant T-Piece Resuscitator
Advantages:
- Delivers consistent set peak inspiratory pressure (PIP)
- Delivers consistent set positive end expiratory pressure (PEEP)
- The operator controls the length of the inspiratory time by varying the duration of time spent occluding the PEEP cap
- Can be used to provide CPAP via a face mask, endotracheal tube or nasopharyngeal tube
- The operator sets the maximum pressure valve and can alter this at any time during operation
- If the operator has achieved a good face mask seal, the pre-set PEEP (usually 5 cmH2O) is displayed on the manometer and an audible soft “whistle” is heard through the PEEP cap. These signs are not seen/heard if there is a leak between the mask and the infant’s face
Limitations:
- Requires a gas source to operate.
- The set PIP (usually 30 cmH2O for a term infant or 20 – 25 cmH2O for a preterm infant) can be reached on the manometer despite a face mask leak of up to 90% (Wood et al, 2008). Visualizing the set PIP on the manometer during ventilation of the infant is therefore NOT an indication of adequate ventilation.
- As the T- piece device delivers a set pressure (as opposed to a set volume) it is still possible to inadvertently deliver large volumes of gas to the infant which may cause a pneumothorax or damage the lungs of a preterm infant.
| In the absence of a respiratory function monitor (e.g. FlorianTM) use heart rate and chest wall movement as a guide to how much PIP you need to adequately ventilate the infant using a T-piece device. |
If the heart rate is below 100/min or decreasing and/or the chest wall is not moving, then increase the PIP in increments of 5 – 10 cmH2O until the heart rate improves.
If the heart rate is above 100/min and the chest wall movement is excessive, then decrease the PIP in increments of 5 cmH2O until the chest wall movement is equal to that seen in normal quiet breathing.
Please review the Operating and troubleshooting a T-piece device (NeopuffTM Infant Resuscitator) presentation on the web site (if you have not already done so) before progressing.
2. Self inflating bag (Laerdal™ or similar )
 Advantages:
Advantages:
- Not dependent on a gas source to function
- Pressures are easy to adjust: simply squeeze the bag harder
- Occluding the pressure relief (“pop off”) valve allows the operator to deliver pressures greater than 40 cmH2O (if higher pressures are required to achieve an increase in heart rate or improved chest wall movement)
- Portable and light weight
- Available in single use, disposable bags
Limitations:
- Does not provide PEEP/CPAP (unless a PEEP valve has been fitted)
- It is difficult to provide consistent inflation pressures
- It is difficult to deliver a sustained inflation longer than 2 – 3 seconds
- Unless an in-line pressure manometer is inserted, the operator does not know how much pressure is being delivered: it could easily be in excess of 40 cmH2O
- Although the maximum pressure is limited to a factory setting of 35 – 40 cmH2O, pressure relief (“pop off”) valves have been shown to activate at a wide range of pressures and well in excess of 40 cmH2O (Ganga-Zandzou, et al, 1996)
- The operator can inadvertently deliver large volumes of gas to the infant which may cause a pneumothorax or damage the lungs of a preterm infant
- When ventilating a newborn infant, clinicians should aim for approximately 4 – 6 mL/kg per breath (e.g. a term infant weighing 4kg requires 16 – 24 mL with each inflation)
- A 240 mL self inflating bag (e.g. Laerdal “preterm” bag) is therefore more than adequate for ventilating any sized newborn infant
| In the absence of a respiratory function monitor (e.g. FlorianTM) use heart rate and chest wall movement as a guide to how hard you need to squeeze the self inflating bag. |
If the heart rate is below 100/min or decreasing and/or the chest wall is not moving, then squeeze the bag a little harder.
If the heart rate is rising above 100/min and the chest wall movement is excessive, then squeeze the bag more gently until the chest wall movement is equal to that seen in normal quiet breathing.
Please review the Operating and troubleshooting a self-inflating bag presentation on the web site (if you have not already done so) before progressing
3. Flow inflating bag (Anaesthetic bag)
Advantages:

- If there is a large leak at the face mask, the bag will deflate, thus alerting the operator that the face mask seal needs to be improved
- Can be used to deliver sustained inflations
- Does provide PEEP
Limitations:
- Requires a gas source to operate
- Able to produce very high pressures, so should ALWAYS be used with an in-line pressure manometer
- More difficult to use without training or experience
Oxygen/air mix (in the absence of a blender)
To blend at 8L/minute
|
Oxygen percentage
|
Oxygen flow (L/min)
|
Air flow (L/min)
|
|
21%
|
0
|
8
|
|
30%
|
1
|
7
|
|
40%
|
2
|
6
|
|
50%
|
3
|
5
|
|
60%
|
4
|
4
|
|
70%
|
5
|
3
|
|
80%
|
6
|
2
|
|
90%
|
7
|
1
|
|
100%
|
8
|
0
|
To blend at 10L/minute
|
Oxygen percentage
|
Oxygen flow (L/min)
|
Air flow (L/min)
|
|
21%
|
0
|
10
|
|
30%
|
1
|
9
|
|
40%
|
2
|
8
|
|
50%
|
4
|
6
|
|
60%
|
5
|
5
|
|
70%
|
6
|
4
|
|
80%
|
7.5
|
2.5
|
|
90%
|
9
|
1
|
|
100%
|
10
|
0
|
Face masks
- Choose an appropriate size mask according to the size of the infant
- The mask should cover the nose and the mouth, but not the eyes
- The mask should not overlap the chin
- Masks with a cushioned rim are preferable to masks without one
- Many commonly available face masks are too large for preterm infants’ faces. A smaller mask of 35 mm diameter is more suitable for an infant <29 weeks’ gestation. (O’Shea et al, 2015).
- Achieving a good seal can be difficult to establish and maintain: just because the mask fits on the face does not mean that the seal is adequate
- Face mask leaks are common, averaging 60%
- Even experienced clinicians can have in excess of 90% leak (Wood et al, 2008)
Reducing face mask leak
- How you hold the mask influences the degree of face mask leak.
- Good face mask technique can be taught and face mask leak can be significantly reduced as a result. (Wood et al, 2008).
- The “two point top hold” ( Figure 1) is one method shown to reduce face mask leak when using a Laerdal round mask.
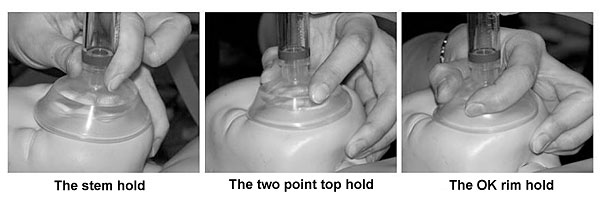
Figure 1: The three hold types demonstrated with the Laerdal round neonatal mask
(Wood, et al., 2008, Archives of Disease in Childhood, Fetal and Neonatal Edition, 93: p. F231)
The technique of mask ventilation
- Place the infant supine with the head in a neutral or slightly extended (“sniffing”) position.
- Do not hyper-extend the head as this will obstruct the airway.
- Open the mouth slightly.
- Briefly suction the airway if there is obvious blood or meconium in the airway (or if secretions obstructing the airway are suspected).
- Inflate the lungs with sufficient pressure and volume that the chest and upper abdomen move slightly.
- The chest movement should equal that seen in normal, quiet breathing.
- Ventilate at a rate of 40 – 60 inflations per minute
- Count: “breathe- two- three, breathe- two- three”, inflating the lungs as you say “breathe” and allowing the infant to exhale on the “two – three”.
Supraglottic airway (SGA)
ANZCOR state:
All personnel who attend births should be trained in newborn resuscitation skills which include basic measures to maintain an open airway, ventilation via a face mask or supraglottic airway (SGA) device and chest compressions. [Good Practice Statement]. (ANZCOR, 2021, Guideline 13.4)
- A supraglottic airway should be considered during resuscitation of the term and near-term newborn (≥34 34 weeks, approximately 2000 grams) if face mask ventilation is unsuccessful. [CoSTR 2015, weak recommendation, low certainty of evidence]
- The supraglottic airway may be considered as a primary alternative to a face mask for positive pressure ventilation among newborns weighing more than 2000 grams or delivered ≥34 weeks’ gestation, although there is insufficient evidence to support its routine use in this setting. [Good Practice Statement]
For more information on insertion and use of a supraglottic airway (also known as a laryngeal mask), see supraglottic airway.
The first breaths of life
- Higher inflation pressures (>30 cmH2O and even as high as 50-60 cmH2O) may be needed for the first few inflations, especially in an infant who has never made any respiratory effort.
- Subsequent inflations usually require less pressure although some infants will require more pressure.
- An infant who gasps will be easier to ventilate with lower pressures than an infant who has never breathed (i.e. whose lungs remain fluid filled).
Assessing the effectiveness of mask ventilation
Effective ventilation will be confirmed by observing the following:
- The heart rate improves and increases to above 100/min
- A slight rise in the chest and upper abdomen with each inflation
- Oxygenation improves
If these signs are not seen, then the technique of mask ventilation needs to be improved.
Consider:
- Is there a good seal between the face mask and the infant’s face?
- Re-apply the mask and create a seal using the “two point top hold”
- Ensure the mask size is suitable for the infant
- Is the infant’s head in the correct position?
-
- Re-position the infant’s head into a neutral or sniffing position
- Are you ventilating with sufficient pressure?
-
- Increase the pressure and see if this makes a difference
- Has the gas supply run out or is the flow rate insufficient?
-
- Check that the cylinders have not emptied and that the flow rate is at least 8 L/min
The preterm infant: special considerations
- Preterm infants establish and maintain functional residual capacity (FRC) when they are ventilated from birth with a PEEP of at least 5 cmH2O. This also helps improve their oxygenation.
- In animal studies, ventilation without PEEP (i.e. with a self inflating bag) resulted in gas entering the distal airways on inspiration, but the distal airways partially collapsed or refilled with liquid at end expiration. (Siew et al, 2009)
To demonstrate the dramatic effect that the application of PEEP has in terms of establishing lung volume and functional residual capacity, you may wish to view the following short videos. These videos have been reproduced with the kind permission of Associate Professor Stuart Hooper and Professor Rob Lewis (and their team) from Monash University, Melbourne, in collaboration with Professor Naoto Yagi of the SPring-8 synchrotron facility in Japan. They have used phase-contract X-ray imaging which allows air to be visualized as it enters the lungs immediately after birth.
Please be aware that the videos are from animal studies using anaesthetised preterm rabbit pups.
Video 1: Positive pressure ventilation without PEEP immediately following birth. Note that despite positive pressure ventilation with a PIP of 35 cmH2O, air only enters the distal airways during inflation. As the distal airways collapse at the end of each inflation, functional residual capacity (FRC) does not increase above the lung’s anatomical dead space.
Video 2: Positive pressure ventilation using a PIP of 35 cmH2O and a PEEP of 5 cmH2O, immediately following birth. Note that within five positive pressure inflations, the distal airways are aerated, lung volume is established and lung volume is maintained (i.e. the distal airways do not collapse at end expiration).
- Animal studies have also shown that preterm lungs can be damaged from large volume inflations within the first six breaths of life. (Bjorkland et al, 1997)
- In the absence of a respiratory function monitor, (e.g. FlorianTM) chest wall movement will have to be used as a guide as to how much pressure is required to move the chest wall adequately, but not excessively.
- Chest wall movement should be equivalent to that seen in normal quiet breathing.
|
Supplemental oxygen during resuscitation
- The normal newborn takes up to 10 minutes of post-natal age to achieve oxygen saturations (SpO2) above 90%.
- There is increasing evidence that even brief exposure to excessive oxygenation can be harmful to the newborn both during and after resuscitation.
- Randomised controlled trials show that commencing resuscitation of a newborn infant with air (21% oxygen) results in a significant reduction in mortality compared to using 100% oxygen. (Davis et al, 2004).
- The use of 100% oxygen for resuscitation of newborns has also been shown to:
- Delay the time to first breath
- Delay the time to first cry
- Cause oxidative stress for up to 4 weeks (Vento et al, 2005)
If you wish to read more about the adverse effects of using 100% oxygen, neonatal mortality and oxidative stress, (particularly in the infant who has suffered a hypoxic ischaemic insult and the preterm infant) please click here.
- Term and near term newborn infants should be resuscitated in air (21%) initially.
- Preterm infants less than 35 weeks’ gestation initially may require up to 30% oxygen to maintain and achieve target SpO2 of 85% at 10 minutes of age. The oxygen concentration can then be adjusted according to the infant’s needs. (Escrig et al, 2008) and (Wang et al, 2008)
- Preterm infants are likely to become dangerously hyperoxic if resuscitated in 100% oxygen.
Supplemental oxygen should be reserved for infants whose condition does not improve during the first minutes after birth. Indications for supplemental oxygen include:
- The infant’s heart rate does not increase to above 100/min despite effective positive pressure ventilation.
- The infant requires external chest compressions as the heart rate is less than 60/min.
- The infant’s heart rate is above 100/min but the infant’s SpO2 is less than 80% at 5 minutes of age or less than 85 – 90% at 10 minutes of age.
ANZCOR state:
“In all cases, the first priority is to ensure adequate inflation of the lungs, followed by increasing the concentration of inspired oxygen only if needed.” (ANZCOR 2016, Guideline 13.4, p.6)
The use of pulse oximetry
ANZCOR (2016, Guideline 13.3) recommend that pulse oximetry is used:
- Whenever the need for resuscitation is anticipated
- When CPAP or positive pressure ventilation is administered for more than a few breaths
- When persistent cyanosis is suspected
- Whenever supplemental oxygen is used
Pulse oximetry should be used to ensure that a newborn infant does not become hyperoxaemic when supplemental oxygen is administered during resuscitation.
The pulse oximeter also provides a continuous display of the infant’s heart rate (if cardiac output and peripheral perfusion are adequate). The infant’s heart rate should be checked intermittently by auscultation with a stethoscope.
Sensor placement:
The oximeter sensor should be placed onto the right hand or wrist as the pre-ductal vessels have better perfusion and oxygenation and also reflects brain stem oxygen delivery (Figure 2).The fastest reading of heart rate (approximately 50 seconds) will be obtained by following these four sequential steps:
- Turn the oximeter on
- Ensure the sensor is not connected to the oximeter cable
- Attach the sensor to the infant’s right hand
- Connect the sensor to the end of the oximeter cable
Figure 2. Pre-ductal pulse oximetry
Factors that affect oxygen saturation measurements following birth include:
- Mode of birth
- Infants delivered by caesarean section take on average two minutes longer to reach a SpO2 greater than 90% compared with those born vaginally. (Kamlin et al, 2006; Dawson et al, 2010)
- Gestational age
- Premature infants take significantly longer to reach a SpO2 greater than 90% compared with term infants. (Kamlin et al, 2006; Dawson et al, 2010)
- Altitude
- SpO2 is significantly higher in infants born at sea level compared with those born at a higher altitude for up to 24 hours after birth. (Gonzales & Salirrosas, 2005)
- Site of probe placement
- Pre-ductal readings (from the right hand) are significantly higher than post-ductal readings soon after birth due to better perfusion, oxygenation and higher blood pressure. By 17 minutes of post-natal age, there is no significant difference between pre and post ductal measurements in uncompromised infants. (Mariani et al, 2007)
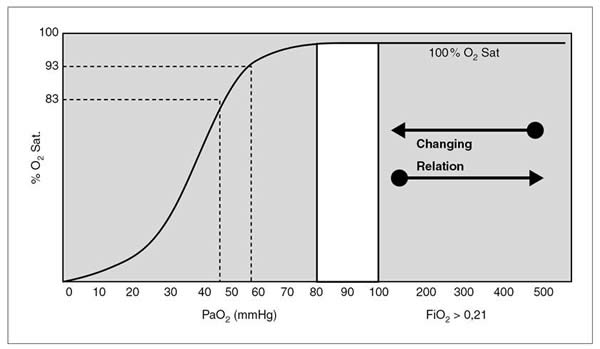
The relationship between SpO2 and PaO2
- Oxygen saturation is the percentage of haemoglobin that is combined with oxygen. Oxygen binding with haemoglobin increases as the partial pressure of oxygen increases, but not linearly. Some neonatal texts describe this relationship using the 30- 60- 90 rule:
- At a PaO2 of 30mmHg, the SpO2 is approximately 60%
- At a PaO2 of 60mmHg, the SpO2 is approximately 90%
- At a PaO2 of 90mmHg, the SpO2 is approximately 95%
- The relationship is more accurately described using the oxygen haemoglobin dissociation curve.
- This is shown in Figure 3 below. Be aware that fetal haemoglobin, hypocarbia, and hypothermia shift the curve to the left, thus hyperoxia can occur at lower saturation levels.
Figure 3: The oxygen haemoglobin dissociation curve
Reference: Sola, Chow & Rogido. (2005). Anales de Pediatria, 62 (3): p. 273.
- The normal range of PaO2 in a newborn infant is 50 – 80mmHg.
- If the newborn is receiving supplemental oxygen, very small changes in oxygen saturation (SpO2) may correlate to significant increases in PaO2. For example, once the SpO2 is 95% or greater, the PaO2 may be well in excess of 100mmHg and as high as 500mmHg: i.e. the infant is dangerously hyperoxic.
- The importance of weaning supplemental oxygen in newborn infants to avoid hyperoxia can not be over-emphasised.
Titrating oxygen to the infant’s requirements
- Studies have shown that extremely preterm infants resuscitated in 100% oxygen will become rapidly hyperoxic. (Tracey et al, 2004; Wang et al, 2008)
- Randomised controlled trials have shown that even extremely preterm infants can achieve a targeted oxygen saturation of > 85% by 7-10 minutes of postnatal age when resuscitation is commenced in low concentrations of oxygen (30 – 40%), thus reducing the oxygen load to the infant. (Wang et al, 2008; Escrig et al, 2008)
- Oxygen should be weaned once the infant’s pre-ductal SpO2 is above 90% (as long as the infant’s heart rate remains above 100 beats per minute).
- Hyperoxia must be avoided.
- Regardless of gestational age, the goal should be to aim for oxygen saturations resembling those of healthy term babies (ANZCOR 2016, Guideline 13.4).
Target saturations for newborn infants during resuscitation
| Time from birth | Target saturations |
| 1 minute | 60 – 70% |
| 2 minutes | 65 – 85% |
| 3 minutes | 70 – 90% |
| 4 minutes | 75 – 90% |
| 5 minutes | 80 – 90% |
| 10 minutes | 85 – 90% |
(ANZCOR 2016, Guideline 13.4, p. 6)
- Supplemental oxygen should be administered if the newborn fails to meet the lower end of these targets.
- Some newborn infants will achieve saturations over 90% without supplemental oxygen.
If you wish to read more about the reference ranges for oxygen saturation in the first ten minutes following birth, please click here.
Key points: |
If the infant is not breathing at birth despite stimulation, then positive pressure ventilation is required.
If the infant’s heart rate is less than 100/min then positive pressure ventilation is required.
A T-piece device, a flow inflating bag, and a self inflating bag are all acceptable devices which can be used to provide positive pressure ventilation.
A positive pressure device which provides PEEP is preferable for a preterm infant.
Air (21%) should be used initially for term and near term infants, with supplemental oxygen reserved for infants whose condition does not improve within the first minutes of life.
Preterm infants less than 35 weeks’ gestation may require up to 30% oxygen initially which can be titrated according to the infant’s oxygen saturations.
Hyperoxia should be avoided, especially in preterm infants.
Using pre-ductal pulse oximetry to guide weaning of supplemental oxygen to avoid hyperoxia, in addition to providing a constant display of the infant’s heart rate.
An increase in heart rate is the primary sign of effective ventilation.
| Previous | Next |